A call away: Virtual physicians offer safe, timely guidance through 8-1-1 line
15 February 2024

Do online doctors provide safe advice? Ross Duncan and researchers wanted to find out.
“During the COVID-19 pandemic, it was difficult to get health care. If you felt ill, visiting a health-care setting in-person could increase your risk of infection,” recalls Ross Duncan, a learning health systems analyst at the BC SUPPORT Unit, Michael Smith Health Research BC (Health Research BC), and adjunct professor at the UBC department of emergency medicine. “Patients needed a safe and timely way to get their health questions answered.”
Many people living in BC struggle to find primary care, and the pandemic made this even more challenging. Without primary care access, people often delay getting help, waiting until their symptoms worsen and need urgent, emergency care.
What you should know
|
|---|
Safely guiding people to suitable care during the COVID-19 pandemic
In 2020, at the height of the pandemic, the number of calls to 8-1-1 rose sharply.
“Callers were asking more complex questions, and about a new disease that hadn’t been studied before. That’s why virtual physicians were added to 8-1-1 in April 2020,” says Ross. “With both virtual nurses and physicians on the line, callers could get more advice on where to seek care.”
But was this new service working? And was it safe?
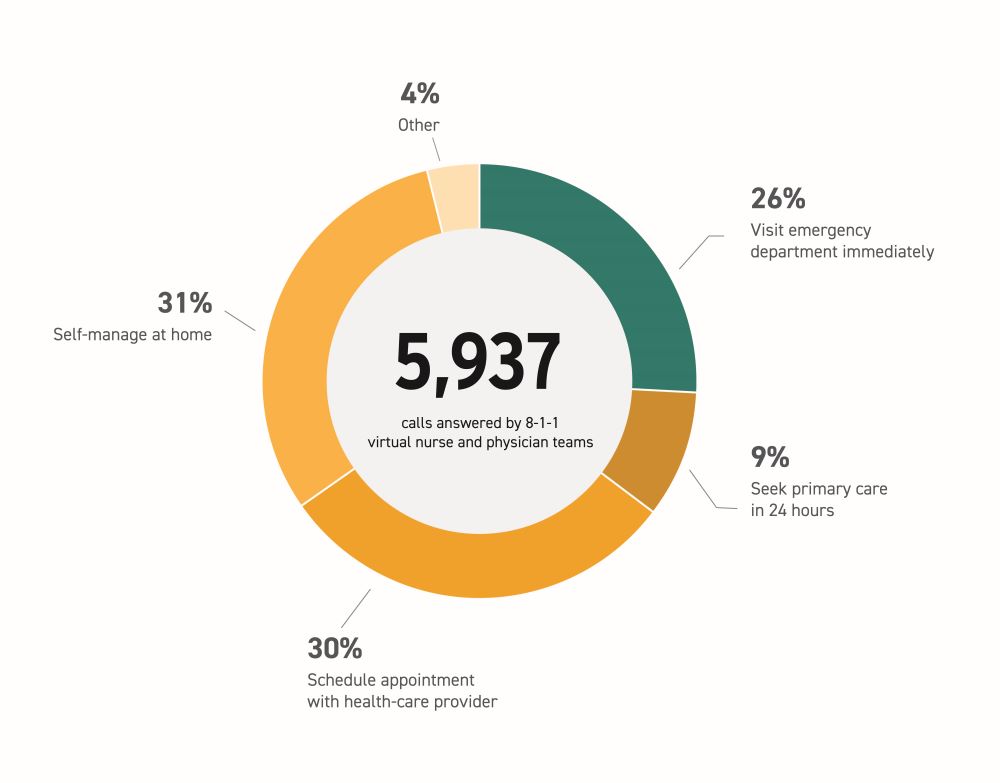
Ross and a group of researchers wanted to find out. From November 2020 to April 20211, they looked at 8-1-1 calls answered by virtual nurse and physician teams. The study was led by researchers at Health Research BC, the UBC department of emergency medicine, the BC Emergency Medicine Network (now Emergency Care BC) and HealthLink BC.
Of almost 6000 calls, only 26 percent of callers were advised to visit the emergency department immediately. The rest were advised to seek less urgent care options. Nine percent were asked to seek primary care within 24 hours and 30 percent to schedule an appointment with a health-care provider. 31 percent were asked to self-manage at home, and of these callers, fewer than three percent were admitted to the hospital in the next week. No patients died.
It was clear that guidance from 8-1-1 nurse and physician teams safely reduced unnecessary in-person visits to the emergency department. They achieved this by redirecting less urgent callers to other care options that still fulfilled their needs.
“Under pandemic conditions, it was crucial that patients could get advice on what they should do for care, before they decided whether or not to make an in-person visit,” says Ross. “The 8-1-1 virtual nurse and physician team helped them do that and get to the right care they needed, without undue risk.”
People in rural and urban areas have different access to health services

After this first study, Ross still had questions. He wanted to know which callers followed 8-1-1 team advice and which ones couldn’t, and why.
In a follow-up study2 led by Ross, researchers looked at what could have influenced a caller’s actions. They looked at factors around the 8-1-1 calls, like time of call, type of advice given and which health services a caller used after 8-1-1. They also looked at information about the callers themselves, like their age, sex and location.
The researchers found that location played a large role in a caller’s ability to follow virtual physician advice.
When callers were advised to visit emergency departments, 70 percent of all callers did so within 48 hours. However, far fewer callers in rural areas followed this advice, compared to those in urban centres. Rural callers might have trouble getting to emergency departments in a timely manner, since most emergency departments are located in urban centres far from rural areas.
By contrast, when callers were advised to seek follow-up care with a family doctor, less than 50 percent of all callers did so in seven days. This trend was more common for callers in urban centres, where fewer people have a family doctor.
“Our research results reflect wider trends of health service use in BC,” says Ross. “We know that in rural regions, people have more difficulty accessing emergency departments, while in urban centres, people have more difficulty accessing family physicians. Identifying these barriers in an 8-1-1 context helps us understand what challenges people are facing, which is the first step to addressing them.”
Access to health data is key
To understand if the new service was working, the researchers needed health data. However, getting access to health data is difficult. Data from health services are stored across multiple organizations, and each one has its own rules for data access and use.
“To get answers, we needed to draw connections between 8-1-1 calls in the province, the callers’ demographic information, and the health services they used. It can be very hard to get that data and to get it quickly,” says Ross.
The researchers were able to access the data they needed through the Health Data Platform BC. The Health Data Platform BC is a secure platform that provides access to health data from multiple organizations. The platform was developed by the Ministry of Health, in partnership with health organizations including the BC SUPPORT Unit. The BC SUPPORT Unit, part of Health Research BC, is a provincial initiative that moves evidence developed with patients into practice.
“The Health Data Platform gave us a single place to access the data we needed, so we could draw those important connections,” says Ross.
In the future, Ross hopes to collect feedback from nurses and 8-1-1 callers, to understand the nurses’ experiences and the callers’ decision-making process.
“We know that people in different areas have different access to health services, but we haven’t yet explored if we can tailor 8-1-1 advice to people living in rural regions and urban centres,” says Ross. “By getting feedback on patient experiences, we hope to strengthen the 8-1-1 service for different communities across BC.”
Learn more about the virtual physician service through 8-1-1, called HealthLink BC Emergency iDoctors in Assistance (HEiDi).
What is the Health Data Platform BC?
- Health Data Platform BC is a secure platform in the cloud, designed for health data research and analysis.
- The results from data analysis can help develop policy, evaluate programs, inform strategy, support academic research and more.
- The platform protects sensitive health data by controlling access, logging and monitoring desktop activity, and reviewing output.
- More information: https://healthdataplatformbc.ca/
References
1 Ho, K., Abu-Laban, R. B., Stewart, K., Duncan, R., Scheuermeyer, F. X., Hedden, L., Lauscher, H. N., Sundhu, S., Chadha, R., Christenson, J., Grafstein, E., Lavallee, D. C., Purssell, R., Tallon, J. M., Wood, N., & Bryan, S. (2023). Health system use and outcomes of urgently triaged callers to a nurse-managed telephone service for provincial health information after initiation of supplemental virtual physician assessment: a descriptive study. CMAJ Open, 11(3). https://doi.org/10.9778/cmajo.20220196
2 Duncan, R., Stewart, K., Scheuermeyer, F. X., Abu-Laban, R. B., Ho, K., Lavallee, D., Christenson, J., Wood, N., Bryan, S., & Hedden, L. (2023). Concordance between 8-1-1 HealthLink BC Emergency iDoctor-in-assistance (HEiDi) virtual physician advice and subsequent health service utilization for callers to a nurse-managed provincial health information telephone service. BMC Health Services Research, 23(1). https://doi.org/10.1186/s12913-023-09821-w





