Health Research BC is providing match funds for this research project, which is funded by the Vancouver Foundation’s Participatory Action Research Investigate Grant.
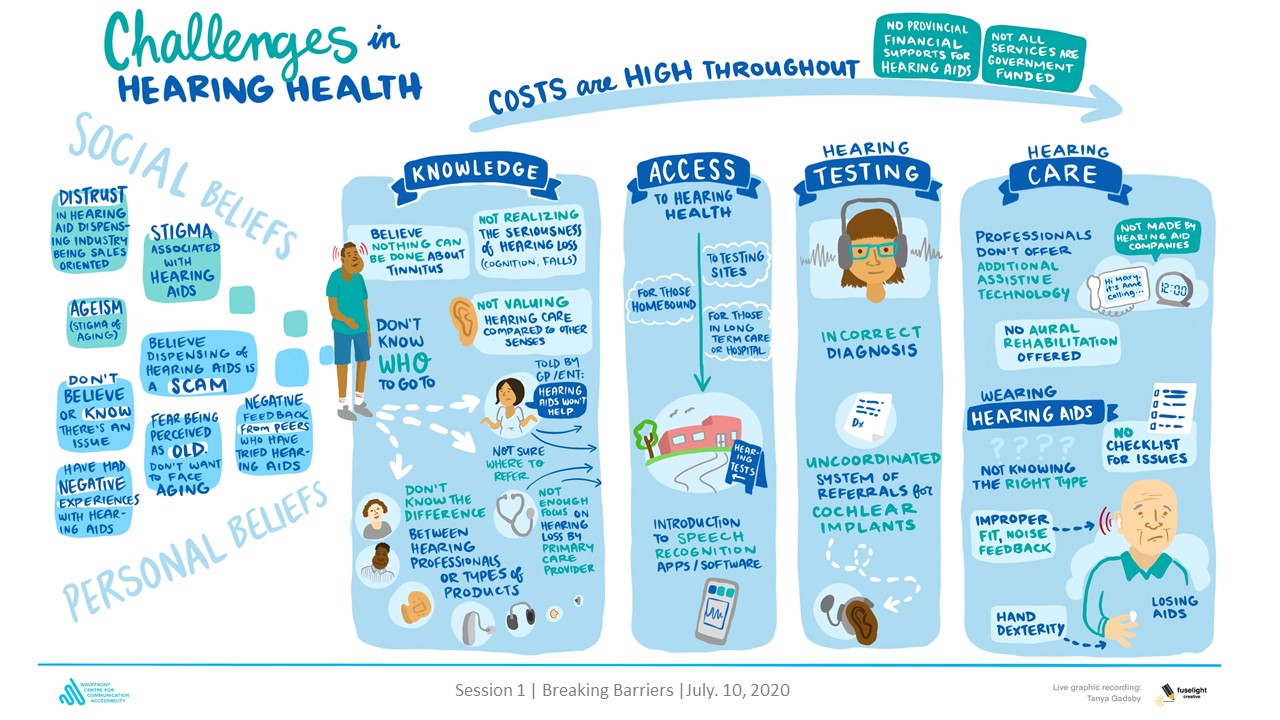
Up to 65% of adults in British Columbia (BC) aged 60+ will develop hearing loss. Fewer than one-quarter of these adults use hearing health care, with most delaying treatment 7 to 10 years on average. Untreated hearing loss affects health-related quality of life with links to social isolation, depression, greater risk of falls, and reduced financial security. For adults with concerns about their hearing, primary care providers (PCPs) are often a first point of contact for help seeking, and yet for reasons that remain unclear, PCP referrals to hearing health care are inconsistently and infrequently practiced. This problem was identified as a top priority through focus groups conducted in 2020. These graphics illustrate the focus group discussions that led to the development of this research question.

We will use a community-based approach to identify reasons for lack of referral and develop strategies that empower primary care providers to be key instigators for increased, timely uptake of hearing health care by individuals with hearing concerns.
The research team, all based in BC, is led by Lorienne Jenstad, PhD, an audiologist and associate professor at the University of British Columbia; Brenda Poon, PhD, the research program lead at the Wavefront Centre for Communication Accessibility; and Ruth Warick, PhD, president of the Canadian Hard of Hearing Association, Vancouver Branch. The team works closely with other individuals who have lived experience of hearing loss, physicians, nurses, clinical audiologists, and community organizations.
Ultimately we hope that primary care providers and the general public will have better recognition of the importance of hearing health and better understanding of the process to receive hearing health services, leading to timely uptake of hearing health care by individuals with hearing concerns and the potential to improve long-term health outcomes.
End of Award Update – February 2025
Results
We were interested in learning how to empower primary care providers (PCPs) to champion hearing health care. Our data collection and partnerships led us to the online platform Pathways BC as the go-to resource for PCPs. We found that Pathways contains very little information about hearing health for adults. Thus, our work can fill an identified gap (providing an algorithm for hearing health care for adults) on a platform that PCPs use regularly in their work.
We learned about systemic barriers to supporting adult hearing health by PCPs. Distrust of audiology (from patients and PCPs) with respect to places that sell hearing aids seemed to lead to a reluctance to make referrals for hearing health care. PCPs noted that time was a factor influencing their referral of patients to hearing health care. As noted by one PCP, discussion of hearing health with the patient would depend on “if I have the time to think of it when the patient did not come in with that specific problem or did not come in for an ear problem.”
Impact
Through our 3-year project, we identified recommendations for promoting hearing health for adults by PCPs in BC, and we developed (with our community advisory group) the content, format, and venue of a hearing health resource for PCPs. We identified that primary care providers hold an important role in promoting hearing healthcare for older adults; yet they encounter multiple barriers to providing optimal hearing health.
Potential Influence
As non-PCPs, we’ve learned about how PCPs navigate the system and how they want to access information, which has led us to explore opportunities for adding hearing-related data fields into electronic medical records in BC.
Next Steps
We will work with the online platform Pathwaysbc.ca that is frequently used by primary care providers in BC to access referral and patient information to finalize a hearing health resource for PCPs.
As identified through our research, the resource should include the following three learning objectives: 1. Identify/implement strategies for optimal communication with patients who have hearing loss; 2. Determine between a referral to an audiologist or ENT; 3. Use a specific validated tool to screen for hearing loss The format of the hearing health resource should be a one-page flowchart to aid in clinical decision making for older adult patients who report hearing concerns The venue for the resource will be the online platform Pathwaysbc.ca
Our plan for the next ~ six months is to finalize the product for primary care providers to access on Pathways BC, develop and deliver several Continuing Professional Development (CPD) sessions for primary care providers to orient them to the new Pathways resource and provide more context.
We will conduct evaluation studies regarding the hearing health resource we have developed for PCPs.

