How do we measure what matters to patients… well?
9 December 2021
Over the last three years through the generous support of CIHR’s Strategy for Patient-Oriented Research, our Patient-Centered Measurement Methods Cluster has partnered with researchers, healthcare providers, patients, and their communities across British Columbia. As the term for our Methods Cluster comes to an end in Spring 2022, we want to highlight what we learned about our stakeholders’ priorities for improving the way we measure what matters to patients.
But first: What is patient-centred measurement?
Patient-centred measurement (PCM) is a scientific approach for obtaining information to help us understand what matters to patients about their experiences with healthcare, and what matters to them about their health.
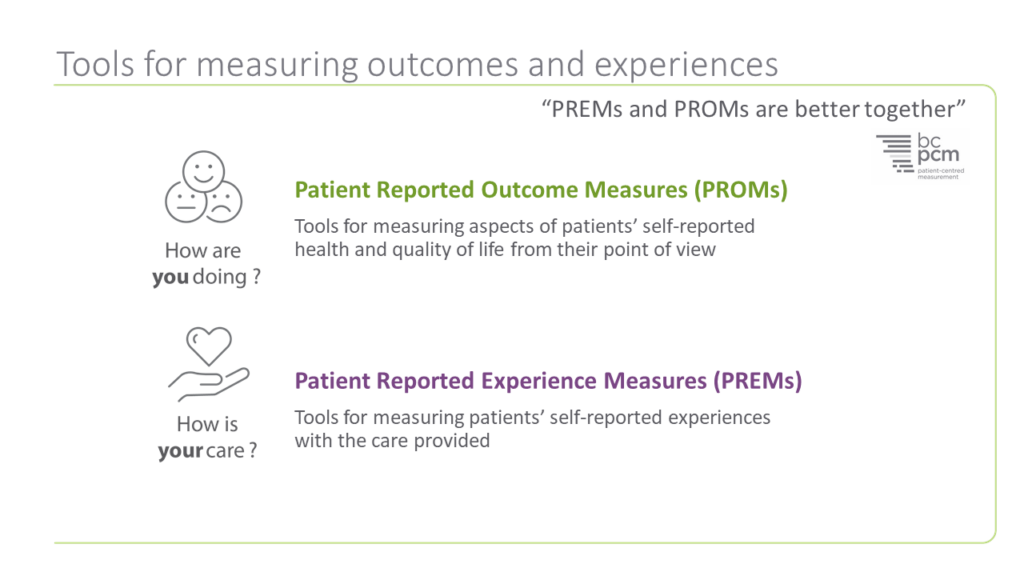
When we do patient-centred measurement well, we capture information that can only be provided by patients themselves — no one else. While the health care system collects a great deal of clinical and administrative data that tells us something about their health conditions and health care, only patients themselves can tell us about their experiences, for example, how they feel about their care, whether they feel (dis)respected by their providers, or how they view their health and quality of life.
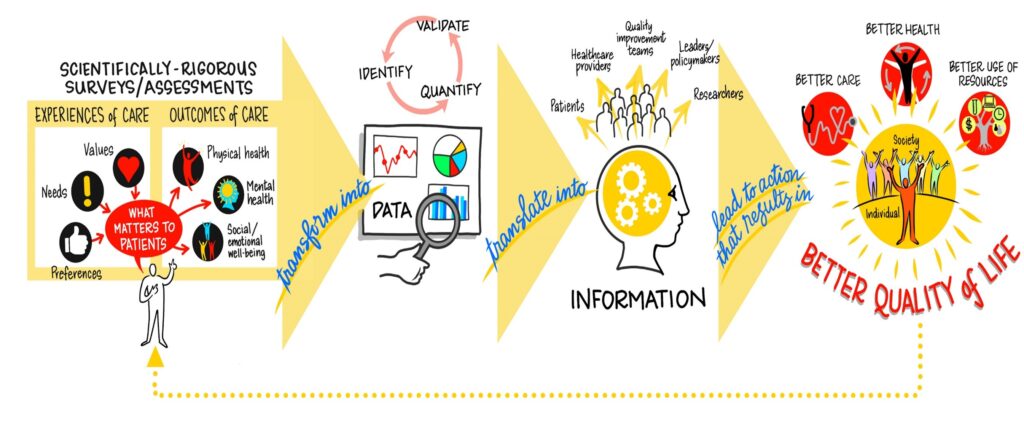
Why care about methods?
Because patient-centred measurement isn’t easy to do! PCM strives to hear from all people: across age, gender, income level, culture, and more — all the ways people differ from one another. We must think about how all these experiences can be represented and accurately captured.
When our measurement methods are not sensitive, inclusive, or safe across our differences, we are not representing diverse perspectives well. For example, when we only provide “male” or “female” response options when asking patients to share information about their gender, we are not providing a measurement tool that collects accurate data, which could lead to decisions that result in flawed and harmful actions.
Further, when our survey questionnaires do not provide space for patients to report mistreatment and harmful practices in their care, the data collected overlooks important information people’s experiences of care. When we fail to ensure our surveys are designed to be listening posts for racism and discrimination where we know it exists, the data tells an incomplete story and by omission does not inform accurate interpretation and appropriate action planning.
How do we solve this problem?
We need to develop better methods and approaches to do patient-centered measurement well. Exactly what our PCM Methods Cluster’s was mandated to do: to advance the science of PCM!
What have we learned so far?
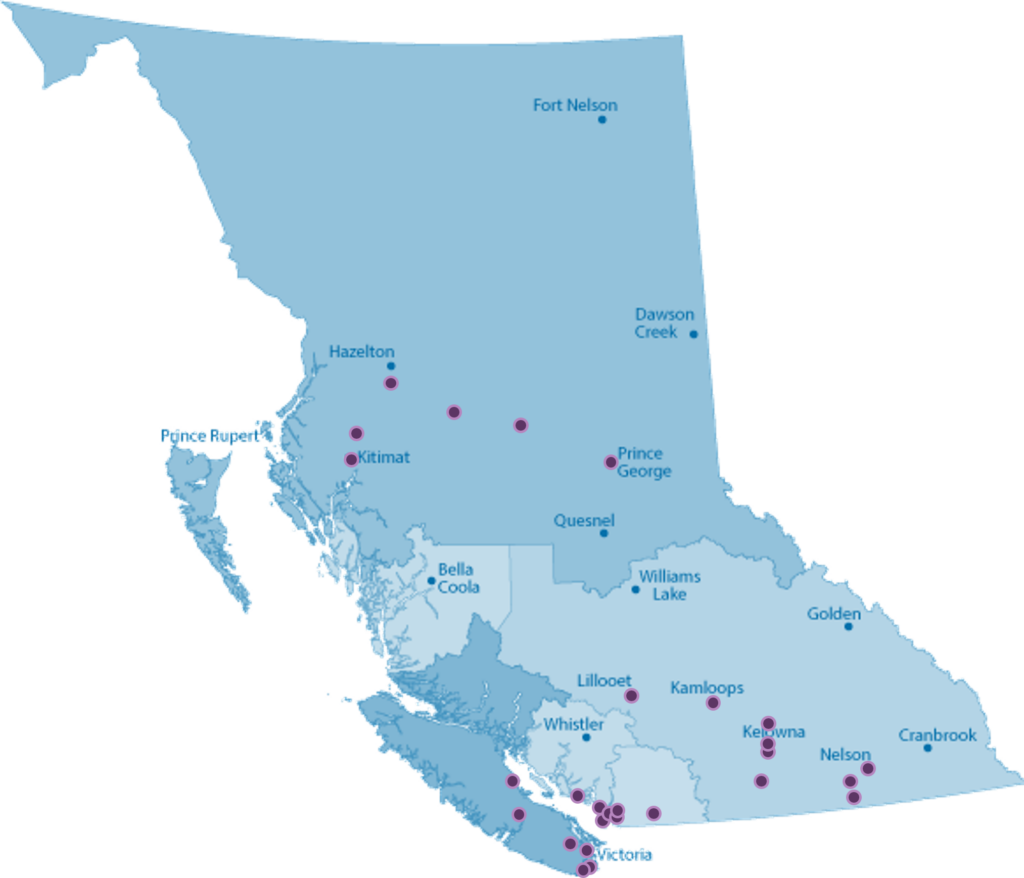
We asked people from across BC about their priorities for developing better ways to measure what matters to them about their experiences with healthcare and about their health. We invited people to participate in focus groups and screened for diversity in gender, age, ethnicity, patient/family caregiver, and urban/rural residence — to try to get as diverse perspectives on priorities for patient-centered measurement as we could. We held seven focus groups with 74 participants across BC’s seven health authorities.
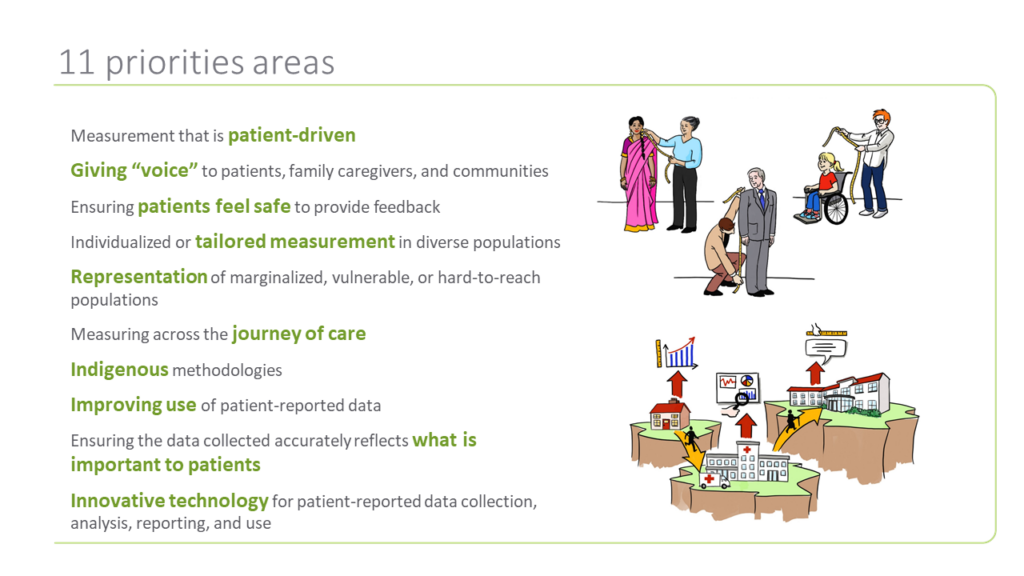
From our focus group learnings — and from the ideas from interviews with 15 subject matter experts and 7 stakeholder workshops (including 94 researchers, clinicians, analysts, and others) — 11 themes emerged.
Download a PDF slide deck of the 11 themes.
Has our PCM Methods Cluster achieved its intended outcome?
We have made a (really) good start! Based on the 11 priority areas that emerged from our engagement with patients, researchers, clinicians, leaders, policy makers and communities across BC, we were able to support 10 research projects that were collaboratively designed with patients and researchers. Several projects are still ongoing. As they become available, results are being made available via project webpages, publications, and webinars.
We are very proud of the engagement that led to the important work of advancing the science of PCM. This work would not have been possible without the funding we received from CIHR and the BC SUPPORT Unit. We owe them and all the patients and researchers who took the time to inform, challenge and co-design the work of the PCM Methods Cluster a huge debt of thanks. Thank you all for joining us on this journey.
Next stop: Integrating and translating the learnings from the 10 PCM Methods Cluster projects into PCM in BC and beyond!
The Methods Clusters project studied the way that patient-oriented research is done, and how it could be better. In a series of blog posts, team members wrote about their work, what they learned and the best ways to engage patients in health research design. The BC SUPPORT Unit provided funding for the project.
This blog post was written by Rick Sawatzky and Lena Cuthbertson.





