A 20-year journey of health research in BC: Voices for patient-oriented research
11 August 2021
Dr. Stirling Bryan and Dr. Saraswathi Vedam
Drs. Stirling Bryan and Saraswathi Vedam: Voices for patient-oriented research
It was an innovative vision to engage patients to improve the health of Canadians through research-based evidence, while improving the cost-effectiveness of the health care system. Backed by the Canadian Institutes of Health Research (CIHR), between January 2009 and August 2010, a 12-member advisory board of pre-eminent voices in health research in Canada gathered to develop the Strategy for Patient Oriented Research (SPOR). One of those voices included MSFHR’s founding President and CEO Dr. Aubrey Tingle, and, following SPOR’s national launch in 2011, MSFHR would play an essential role in leading the development of a BC-focused patient-oriented research unit to provide local support to both the health research and patient community.
In BC, experienced health economist Dr. Stirling Bryan, then Director of the Centre for Clinical Epidemiology & Evaluation at VCH Research Institute and professor at UBC’s School of Population and Public Health, followed the news with interest. Having been recruited to Canada in 2008 to support and focus on policy-relevant research, he was interested in understanding the policy changes needed to shift patients from being passive receptors of health research to becoming proactive partners in work that could help them. In 2014, along with 26 other BC health research centre leads and many other health system contributors, he provided expertise on existing BC health research capacity, and later joined the proposed provincial unit’s business plan development team, led by MSFHR.
The clinician researchers reflected that supporting patient autonomy requires bringing a patient’s stated values into care planning — not as a single event, but as an ongoing process.
The resulting BC SUPPORT Unit (Support for People & Patient-Oriented Research & Trials Unit) plan represented a provincial commitment to a fundamental change in the way BC set priorities for, conducted and applied health research — and how, collectively, the health sector, the BC community and the research sector would support continuous learning from these efforts. In 2015, CIHR approved the Unit’s business plan and a year later Stirling took on the role of Scientific Director for the Unit.
Reflecting on the changes in the health research community since SPOR and the BC SUPPORT Unit were established, Stirling says, “We have made significant progress and the culture is changing. Some research teams have fundamentally changed how they operate.”
In particular, he points to the BC SUPPORT Unit’s Methods Clusters projects as examples of how to conduct research focused on improving our understanding of the best ways of doing patient-oriented research. One of these 42 projects in progress includes Decolonizing birth research: Indigenous researchers, clinicians and community experts measuring respect, disrespect and mistreatment in Indigenous childbearing communities. This Indigenous-researcher-led project aims to develop person-centred measures of respect, disrespect, racism and/or mistreatment as experienced by Indigenous families during pregnancy and childbirth. Indigenous Knowledge Keepers and Elders will provide leadership throughout the project to ensure that Indigenous ways of knowing drive Indigenous ways of doing. The study is led by Indigenous researchers: Dr. Rachel Olson, Co-Director of The Firelight Group, and Dr. Wanda Phillips-Beck, Seven Generations Scholar, with the support of Elder Roberta Price and Dr. Saraswathi Vedam, a passionate patient advocate, registered midwife and MSFHR awardee.
“I have learned from my Indigenous colleagues,” Saraswathi says. “They are saying: now is the time to honour those stories. For all the troubling stories, there are stories of amazing, kind and supportive care provided by all types of providers. We need to put the focus on these insights, instead of the health system’s needs, to learn how to be better.”
Understanding the diverse needs of patients and advocating for their voices has always been a focus for Saraswathi. As a child, she looked up to her family members who cared for affluent populations in India, but also took care of communities where it was needed — the slums of Mumbai and Chennai. “My mother’s sister was a teaching midwife, my grandfather was a family physician and I had three aunts who were obstetrician-gynecologists (OB-GYNs). I was exposed to maternity care and care of marginalized populations growing up.”
In the early 1980s, Saraswathi pursued the then-uncommon nurse midwife masters degree at Yale University. Upon graduating, she found the health care system in the US fragmented, and clientele with diverse socio-economic backgrounds were looking for continuity of care and support during a life-changing experience. Health care policy and licensing contributed to the stress that new parents and care-providers had to endure, with licensed midwives having to choose between providing home birth or hospital births, or pre-partum or postpartum care. Deemed a Class D felony in some states, direct-entry midwives offering community-based care was in the same category as arson or armed robbery.
Undeterred, after getting her licence and practicing for several years in New York and California, Saraswathi moved to Indiana with her family and opened a home office in Indianapolis. For seven years, she was the only midwife in the state who was licensed, accepted state-supported Medicaid insurance, and legally able to offer a place-of-birth option to new parents. She was also the only midwife of colour, and expecting parents drove hours to see her, seeking cultural safety and to have some autonomy in how birth would happen. It was an experience she wouldn’t soon forget, and she kept an annotated bibliography of readings about patient-focused care that resonated with her.
“Patient partners help us as researchers to see things we may not have thought of. We need to be open to listening to these stories and seeing new ways forward.”
In 2012, Saraswathi had closed her practice in Indiana to take on a faculty role at Yale University, teaching incoming midwives how to provide evidence-based antenatal and intrapartum care across practice settings. Subsequently, when she was recruited to Vancouver to be the Director of the Midwifery Program, Faculty of Medicine at UBC, she brought her Birth and Beyond midwifery practice to BC.
“I never intended to be a researcher,” Saraswathi says, smiling as she remembers joining the well-published UBC faculty team that included researchers Dr. Eileen Hutton and Dr. Patti Janssen. “I learned that when you are a clinical researcher, you can apply the realities of practice to ask the questions that need to be asked, or seek solutions that are person-centred and focused on what they need — as opposed to what the system needs or the provider’s needs are.”

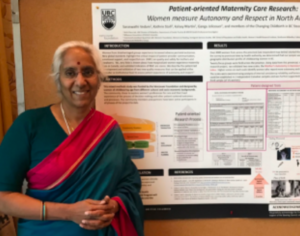
In 2014, Saraswathi and her team led Changing Childbirth in BC, the first province-wide study to try to understand experiences of childbearing care. The study’s topics and questions were chosen by patient partners from diverse and disadvantaged community groups, including recent immigrants and refugees, formerly incarcerated women, rural service users and people from historically marginalized populations. The participatory study was a success, with over 4,000 respondents providing survey data that helped create two evidence-based tools that measure respect and autonomy in maternity care. The Mothers on Respect Index (MOR) and the Mothers Autonomy in Decision Making scale (MADM) are now used in research and to improve care internationally.
Based on the overwhelming response to the project, it was clear that additional support was needed to help share the findings back with the community and translate the data into practice. In 2017, Saraswathi was awarded the MSFHR Health Professional-Investigator award, providing funding for knowledge translation for the project. This funding helped the Changing Childbirth team share the findings back with the women who had shared their stories through video clips, social media graphics and a performance with a Talk Back session to foster further discussion.
MSFHR funding also helped Saraswathi and her Birth Place Lab team provide evidence and recognition of the standards for quality of care during pregnancy, during birth, and after birth, emphasizing not just physical outcomes, but also a person’s psychosocial experiences. Reporting out on the Changing Childbirth study findings, the team conducted and published content analyses of 1,540 written accounts from women in BC who reported on their experiences of declining tests or procedures during pregnancy or childbirth. These studies represent the first and largest analysis of BC data on patients’ experiences when they decline tests or procedures during pregnancy or childbirth. Some had procedures conducted without their consent and/or experienced coercion, disrespect or extreme pressure to accept interventions, and others reported respect and supportive, kind acceptance and exceptional care. Participants described not having choice and experiencing a lack of respect when asserting their autonomy as reducing their self-efficacy, mental health and willingness to engage with health care in the future. The clinician researchers reflected that supporting patient autonomy requires bringing a patient’s stated values into care planning — not as a single event, but as an ongoing process. These experiences are greatly influenced by interactions with health care providers — including physicians, midwives and nurses — and factors such as respect, trust, agency and autonomy have emerged as critical aspects of quality maternity care.
Finding a way to bridge the gap between policy and practice through patient-informed research continues to be a focus for Saraswathi. In 2018, she convened a multi-stakeholder research team that included a steering council of patient partners to study respectful maternity care across Canada in the CIHR-funded RESPCCT study. Over 5,000 people across various identities, circumstances and backgrounds have contributed to date. In recent years, she has given back to the maternity care system in the U.S. by working to change legislation through the historic Home Birth Summits that brought together physicians, midwives, hospital administrators, legislators, liability specialists and more to discuss how to provide equitable, safe, high-quality maternity care to communities and birth place settings across the country. “Birth is a healthy event in a person’s life that needs a medical view in case something goes wrong,” she says. “We’re working to make this common knowledge.”
Like Saraswathi, this approach to thinking about how to improve policy and care from those with lived experiences is one that Stirling also knows well and advocates for. In 2016, the BC SUPPORT Unit became part of the newly established BC Academic Health Science Network (BC AHSN) and in 2020, Stirling assumed the role of President of BC AHSN. Just as Saraswathi does in her work, he continues to push to incorporate patient voices where needed. “Patient-oriented research still needs some thought,” he says. “Patient partners help us as researchers to see things we may not have thought of. We need to be open to listening to these stories and seeing new ways forward.”
Learn more:
Strategy for Patient-Oriented Research – CIHR
BC SUPPORT Unit (Support for People & Patient-Oriented Research & Trials Unit)
MSFHR 2017 Health Professional-Investigator Award: Women Taking Charge of Changing Childbirth in BC
Changing Childbirth in British Columbia: Final Report
Publications supported by Dr. Vedam’s MSFHR award:
I felt so much conflict instead of joy: an analysis of open-ended comments from people in British Columbia who declined care recommendations during pregnancy and childbirth. (Stoll et al, Reprod Health, April 2021)
I fought my entire way: Experiences of declining maternity care services in British Columbia (Niles et al, PLOS One, June 2021)